01 / 03
HYLO GEL®
by Ursapharm
IntroductionMedication Usage
Hylo Gel®
Insufficient Tears and Tear Film Dryness
Sincerely recommend to those who experience the following issues
-
Deep hydration
-
Dry eyes
-
Burning sensation
-
Eyestrain
-
Foreign body sensation
What is Hyaluronic Acid?
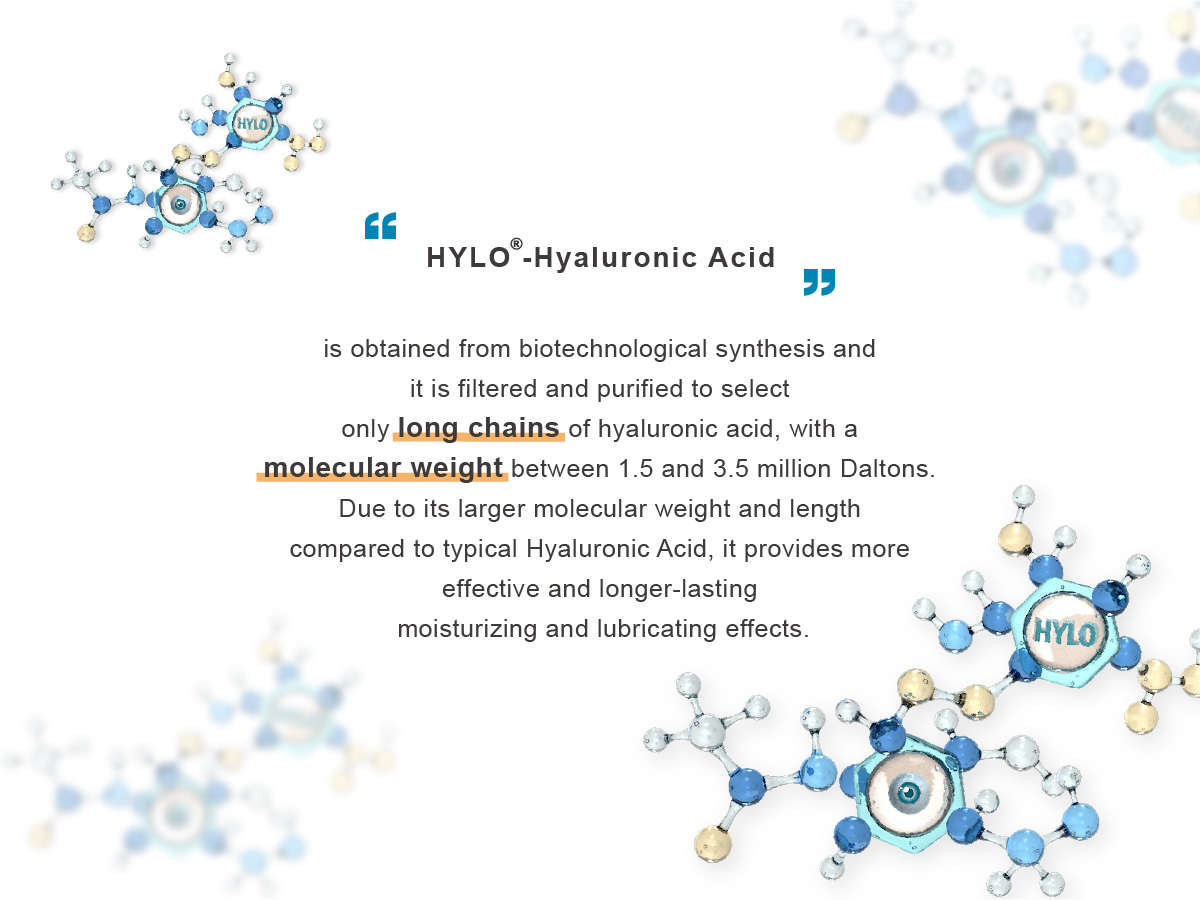
Hyaluronic Acid is a highly effective moisturizing factor and a substance naturally produced in the human body. It is particularly abundant in the eyes and joints, where the liquid has the highest concentration of Hyaluronic Acid.
This hydrophilic molecule can hold a large amount of water and carry water that is 1000 times its own weight.Each blink forms a protective film for the eyes, providing long-lasting hydration, nourishment, and fatigue relief.
Due to the high binding capacity of hyaluronic acid with water and the high physical-chemical similarity with the glycoproteins of the corneal mucosal layer, it has an excellent ability to bond to the ocular surface, performing the following actions on the eye in case of suffering from Dry Eye:
- Hydration, moisturization, and fatigue relief
- Improvement of corneal epithelial cell condition
- Enhancement of tear film stability
Hylo Gel® Ingredient Information
- Sodium hyaluronate 2 mg/ml
- Preservatives-free
- Phosphate-free
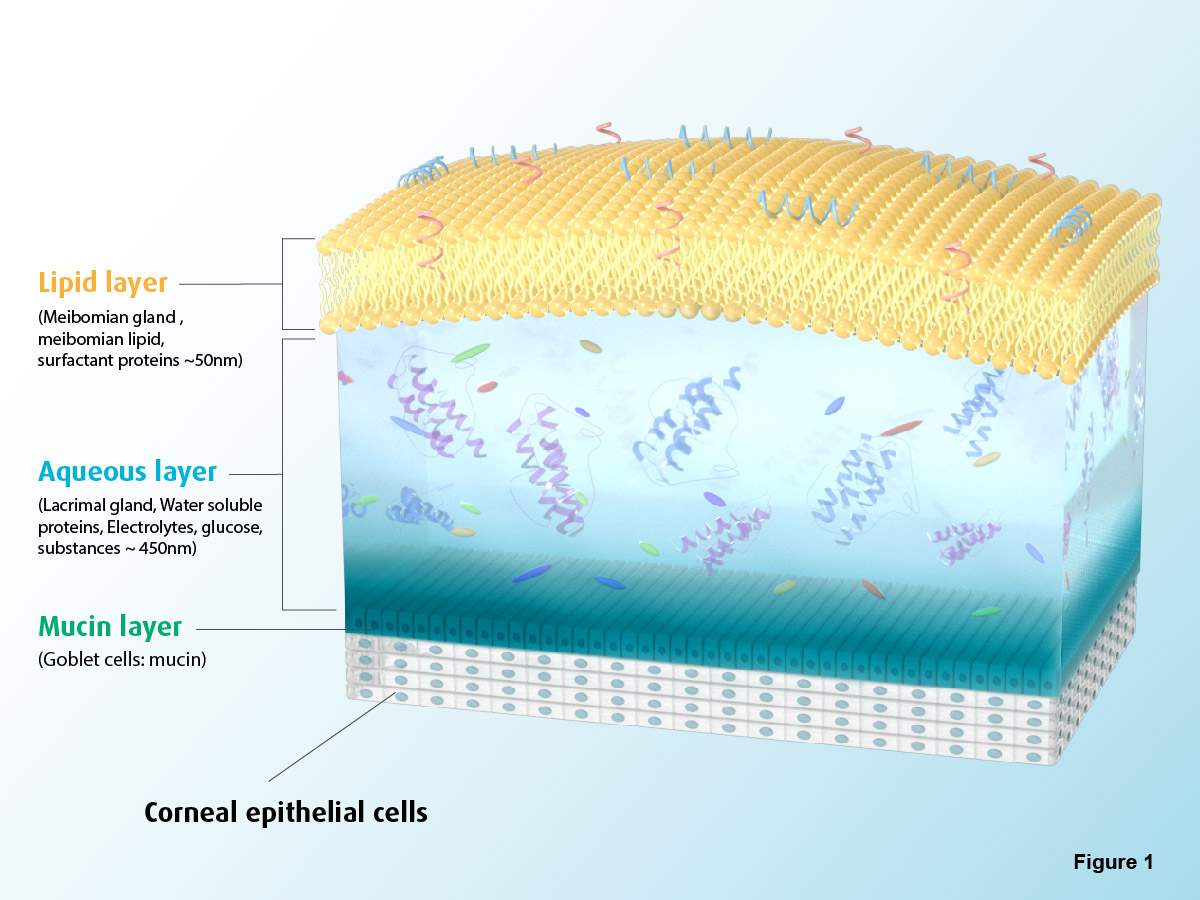
- Image 1: Structure of Normal Tear Film
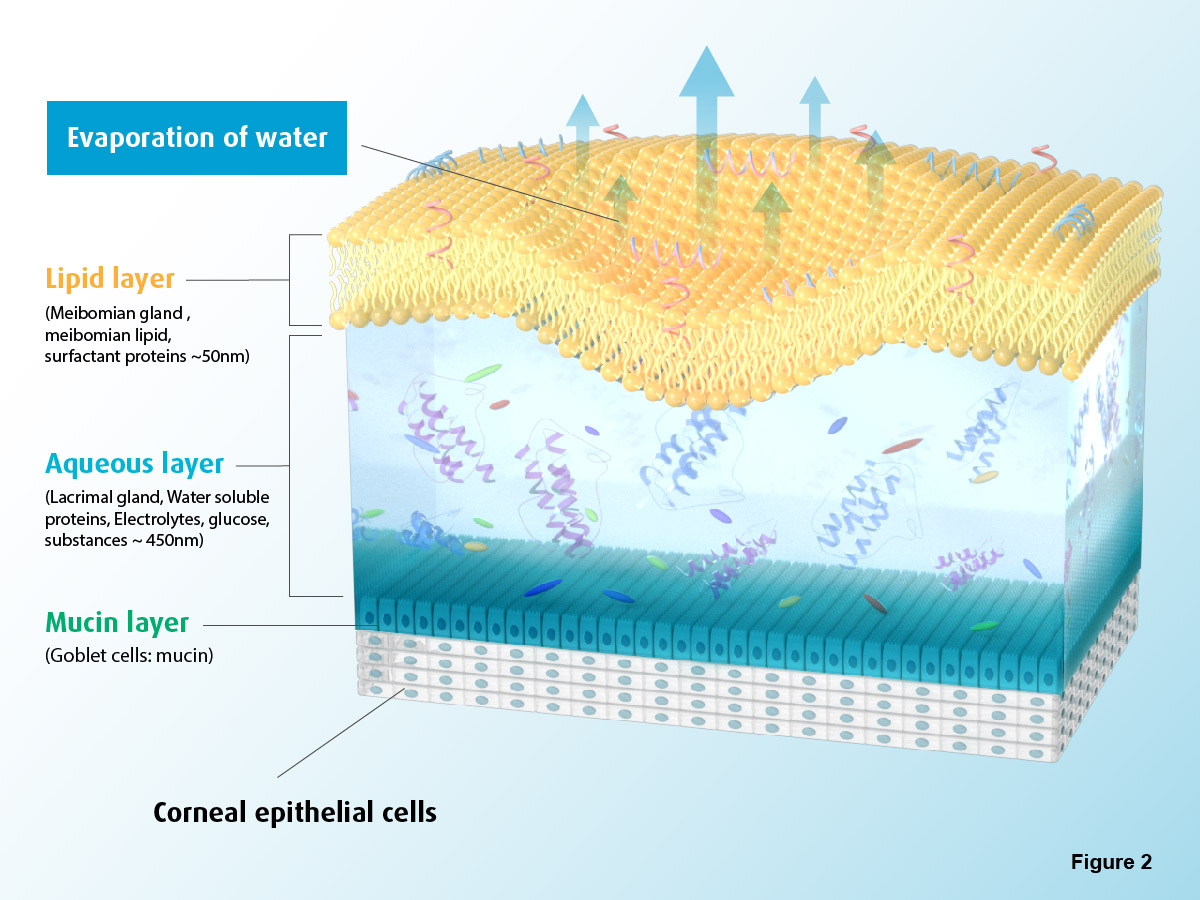
- Image 2: Structure of Tear Film breakup
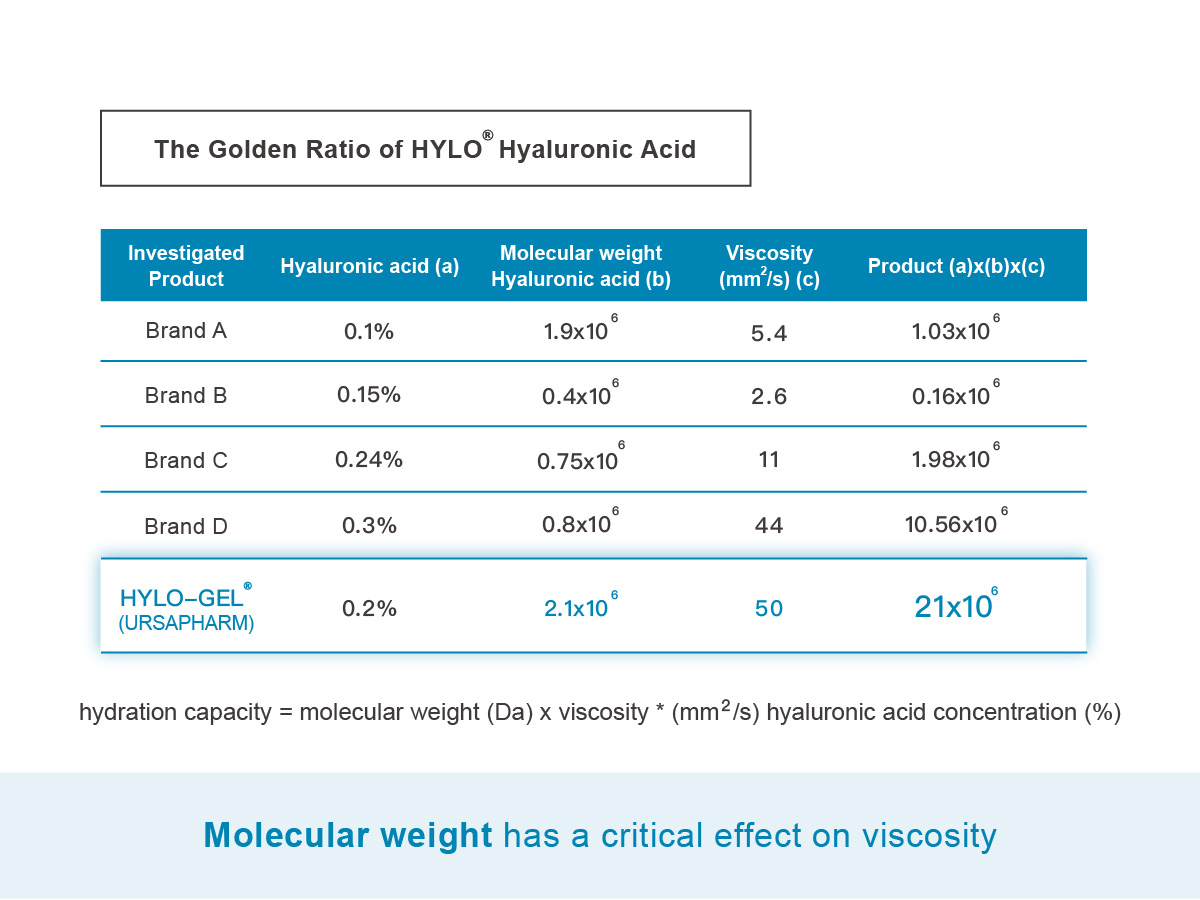
Experience the difference with HYLO® Hyaluronic Acid!
Comod system is the new future for your eyes

The Patented System
Hylo®-Gel supplied in bottles with the patented COMOD® system.

Preservatives Free
The negative pressure created pulls and the flexible inner sachet more. The inner sachet stays sealed and the liquid is protected against contamination from the air.

Can be used 6 months after opening
The contents remain sterile for a period of use of 6 months.

Drop-by-drop dosage
The COMOD® dosage system makes it possible to dispense exactly one drop per pump stroke.

Compatible with contact lenses
The preserved eye drops can stick to the contact lens material and preservatives can lead to a toxic response on the ocular surface.
Friendly Reminder: Before using this product, please consult a specialist or professional healthcare provider if you are an infant, child, or pregnant woman.